Diabetes Management
Do You Have Frequent Infections? It Could Be A Sign Of Diabetes
7 min read
By Apollo 24|7, Published on - 22 August 2023
Share this article
0
0 like

Frequent infections can be a cause for concern, as they could potentially be a sign of an underlying health condition. One such condition is diabetes, which has been found to increase the risk of developing various types of infections. In this blog, we will explore the connection between diabetes and frequent infections, including yeast infections, urinary tract infections (UTIs), skin infections, diabetic foot infections, and diabetic ketoacidosis.
How Infections are Linked to Diabetes?
Diabetes is a metabolic disorder characterized by high blood sugar levels. These elevated sugar levels can have detrimental effects on the immune system, making individuals with diabetes more susceptible to infections. Here's how it works:
1. Weakening of immune response
High blood sugar levels can impair the function of various immune cells, such as neutrophils and macrophages, which are responsible for fighting off infections. This weakened immune response can make it harder for the body to control and eliminate bacteria, viruses, and fungi.
2. Impaired wound healing
Diabetes can also impair the body's ability to heal wounds effectively. High blood sugar levels can damage blood vessels and nerves, leading to poor circulation and decreased sensation in the extremities. This can result in delayed wound healing and increased susceptibility to infections, particularly in the feet, which is a common complication known as diabetic foot infections.
Specific Infections Associated with Diabetes
Some of the common infections associated with diabetes include:
- Urinary Tract Infections (UTIs): High blood sugar levels create an ideal environment for bacteria to thrive in the urinary tract, leading to frequent infections.
- Skin Infections: Diabetes can affect the skin's ability to heal properly, making individuals more prone to skin infections. Common skin infections in individuals with diabetes include cellulitis (a bacterial infection) and fungal infections.
- Respiratory Infections: Individuals with diabetes are more susceptible to respiratory infections, such as pneumonia. High blood sugar levels can weaken the immune system and impair lung function, making it harder for the body to fight off respiratory infections.
Signs and Symptoms of Diabetes-Related Infections
Some of the common symptoms of infections associated with diabetes include:
- Increased susceptibility to infections: If you find yourself getting infections more frequently than usual, especially UTIs, skin infections, or respiratory infections, it could be a sign of underlying diabetes.
- Delayed healing of wounds or sores: Wounds or sores that take longer to heal than usual may be a result of compromised immune function due to high blood sugar levels.
- Recurrent or persistent infections: If you keep getting infections that keep coming back despite appropriate treatment, it is important to consider diabetes as a possible underlying cause.
Diagnosing Diabetes and Associated Infections
When it comes to diagnosing diabetes and associated infections, various tests can help determine the root cause of frequent infections.
1. Blood glucose tests for diabetes diagnosis
The primary test for diabetes diagnosis is a blood glucose test (fasting, post-prandial, or random), which measures the level of sugar in the blood. If your blood glucose levels are consistently high, it may indicate that you have diabetes.
2. Additional tests to identify specific infections
In addition to blood glucose tests, other tests that can help identify specific infections linked to diabetes include:
- Urine culture: This test examines a sample of your urine to check for the presence of bacteria. It can identify urinary tract infections, which are common in people with diabetes.
- Blood culture: This test involves taking a sample of your blood and testing it for the presence of bacteria or other microorganisms. It can help detect bloodstream infections, such as sepsis or cellulitis.
- Skin swabs or biopsy: These tests involve taking a sample from an infected area on the skin and testing it for the presence of bacteria or fungi. They can help diagnose skin infections like cellulitis or fungal infections.
- Imaging tests: In some cases, imaging tests such as X-rays, CT scans, or ultrasounds may be necessary to identify infections in deeper tissues or organs.
Managing and Preventing Infections in Diabetes Patients
Measures that may help prevent and manage infections in diabetics include:
1. Controlling Blood Sugar Levels
A. Importance of regular monitoring: Regular monitoring of your blood sugar levels is essential for keeping them within a healthy range. This can be done at home using a blood glucose meter or through regular check-ups with your healthcare provider.
B. Medication management (insulin or oral medications): It's also important to follow your medication regimen as prescribed, whether it's insulin injections or oral medications.
2. Strengthening the Immune System
A. Healthy lifestyle habits: Make sure to maintain a balanced diet, rich in fruits, vegetables, whole grains, and lean proteins. Regular exercise helps keep your immune system strong, therefore, you must engage in physical activity for at least 30 minutes a day. Additionally, managing stress through relaxation techniques like meditation or yoga can also support a healthy immune system.
B. Vaccinations for preventable infections: Vaccinations for illnesses like the flu and pneumonia are highly recommended for individuals with diabetes. These vaccines help protect against preventable infections that can further weaken the immune system.
3. Proper Wound Care and Hygiene Practices
A. Importance of regular foot care for diabetic patients: Proper wound care and hygiene practices are essential for individuals with diabetes. Diabetic patients should pay extra attention to their feet and practice regular foot care to prevent infections.
B. Guidelines for wound cleaning and dressing: If you do develop a wound or infection, proper care is vital to prevent further complications. Follow these guidelines:
- Clean the wound gently with mild soap and water.
- Use an antiseptic solution recommended by your healthcare provider.
- Apply an appropriate dressing to protect the wound and promote healing.
4. Nutritional Recommendations to Boost Immunity
A. Foods to include in a diabetes-friendly diet
Include a variety of fruits and vegetables, choose whole grains, consume lean proteins, and limit processed foods and added sugars.
B. Indian-specific dietary suggestions
- Incorporate traditional Indian spices such as turmeric, ginger, and garlic into your meals. These spices have anti-inflammatory properties that can help strengthen your immune system.
- Include regional fruits and vegetables that are rich in nutrients. For example, gooseberries (amla), drumsticks (moringa), and bitter gourd (karela) are known for their immune-boosting properties.
- Opt for healthier cooking methods like steaming, grilling, or stir-frying instead of deep frying.
C. Treatment Options for Diabetes-Related Infections
Usually, the treatment for diabetes-related infections includes:
- Antibiotics for bacterial infections: Your doctor will prescribe the appropriate antibiotic based on the type and severity of the infection. It is essential to complete the full course of antibiotics as prescribed, even if you start feeling better before completing the treatment.
- Antifungal medications for fungal infections: Fungal infections, such as oral thrush or vaginal yeast infections, may require antifungal medications. These medications can be in the form of creams, ointments, or oral tablets. It's important to follow your doctor's instructions and complete the entire course of treatment.
When to Consult a Doctor?
Signs you need consultation from a doctor include:
1. Persistent or severe infections: If you have an infection that doesn't seem to go away or worsens over time, it's essential to consult a doctor. This could be a sign that your body's immune system is compromised, making it difficult to fight off the infection effectively.
2. Uncontrolled blood sugar levels: High blood sugar levels can weaken your immune system, making you more susceptible to infections. If you are struggling to control your blood sugar levels despite your best efforts, consult a diabetologist.
Conclusion
Remember, early detection and timely treatment of infections are crucial for individuals with diabetes. If you notice any signs of infection, do not hesitate to seek medical help. By taking the necessary precautions and following your doctor's advice, you can effectively manage diabetes-related infections.
Consult Apollo's Expert Diabetologists
FAQs
Q. Why are diabetic foot infections a concern?
Poor circulation and nerve damage in the feet can lead to foot ulcers that are slow to heal and prone to infection.
Q. Are there any specific vaccines recommended for people with diabetes?
Yes, it is recommended that diabetics receive vaccines for influenza, pneumococcal disease, and hepatitis B.
Q. Why do urinary tract infections occur more frequently in people with diabetes?
High blood sugar levels provide an ideal environment for bacteria to grow in the urinary tract.
Q. What is diabetic ketoacidosis (DKA) and why is it a concern?
DKA is a serious complication of diabetes characterized by high blood sugar levels and the presence of ketones. It can lead to a life-threatening condition if not treated promptly.
Q. Can diabetes affect oral health and increase the risk of dental infections?
Yes, diabetes can increase the risk of gum disease, tooth decay, and oral infections.
Diabetes Management
Consult Top Diabetologists
View AllLeave Comment
Recommended for you

Diabetes Management
A Step-By-Step Guide To Using A Glucometer
Regular blood sugar monitoring is crucial for effective diabetes management. Glucometers, portable devices that measure blood glucose levels at home, offer convenience. To use a glucometer, start by gathering necessary supplies: soap or alcohol prep pads, test strips, a lancing device with a new lancet, and a notepad or smartphone app to record results. Follow these steps: clean your hands, turn on the glucometer, prick your fingertip, apply blood to the test strip, stop bleeding, and record the results.

Diabetes Management
Insulin Therapy for Diabetes: Separating Myths from Facts
Insulin treatment may not lead to weight gain. In type 2 diabetics, undergoing insulin treatment, weight gain is frequently caused by the improved blood glucose control and higher effectiveness in utilising glucose. Insulin itself does not directly cause it. The initial weight increase frequently stabilises with time, proper diet and exercising.
Diabetes Management
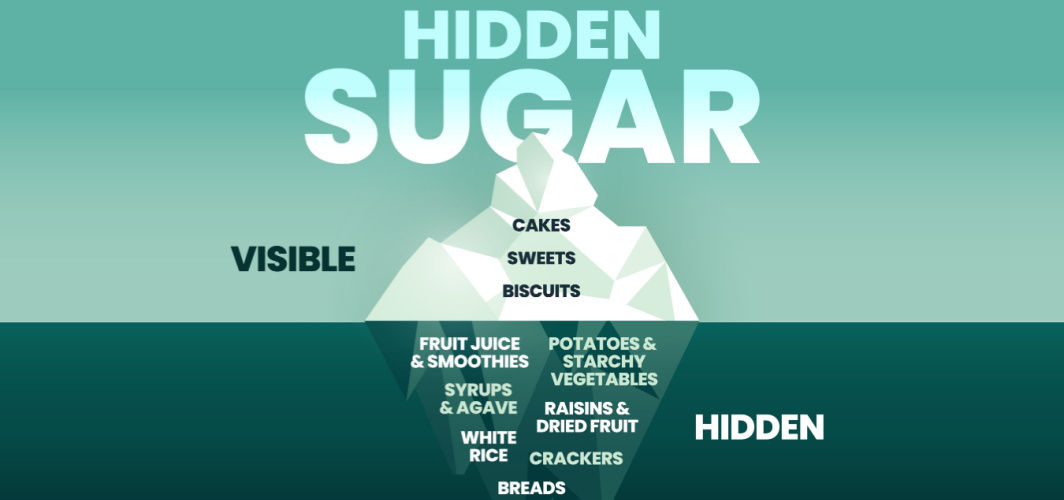
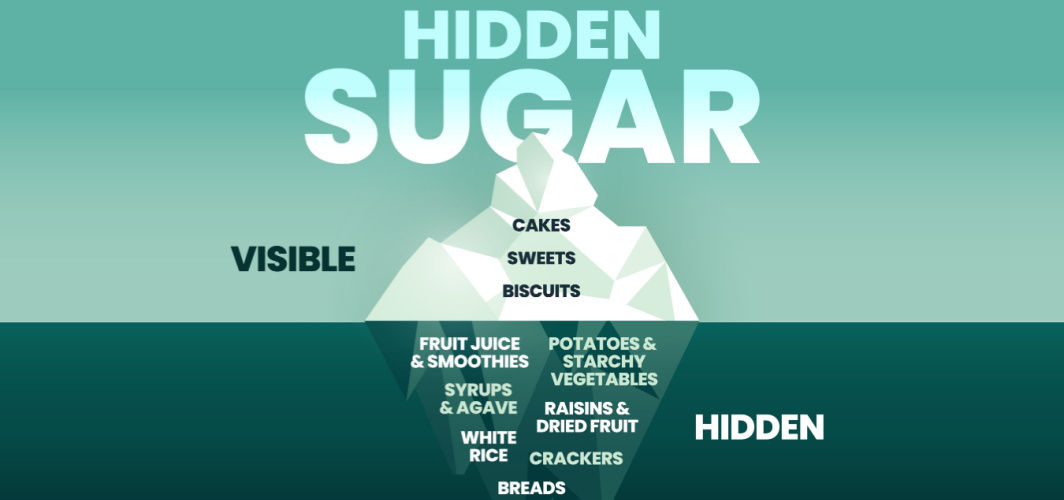
Avoid or Limit These Common Foods with Hidden Sugar
Some foods that may contain hidden sugars include flavoured yoghurt, granola bars, canned fruit in syrup, condiments like ketchup and barbecue sauce, flavoured coffee drinks, packaged sauces and dressings, certain breakfast cereals, and processed snacks. Diabetics should read the food labels and be extra cautious about ingredients to manage diabetes well.
Subscribe
Sign up for our free Health Library Daily Newsletter
Get doctor-approved health tips, news, and more.
Visual Stories

8 Fruits That are Incredibly Healthy for Diabetes
Tap to continue exploring
Recommended for you

Diabetes Management
A Step-By-Step Guide To Using A Glucometer
Regular blood sugar monitoring is crucial for effective diabetes management. Glucometers, portable devices that measure blood glucose levels at home, offer convenience. To use a glucometer, start by gathering necessary supplies: soap or alcohol prep pads, test strips, a lancing device with a new lancet, and a notepad or smartphone app to record results. Follow these steps: clean your hands, turn on the glucometer, prick your fingertip, apply blood to the test strip, stop bleeding, and record the results.

Diabetes Management
Insulin Therapy for Diabetes: Separating Myths from Facts
Insulin treatment may not lead to weight gain. In type 2 diabetics, undergoing insulin treatment, weight gain is frequently caused by the improved blood glucose control and higher effectiveness in utilising glucose. Insulin itself does not directly cause it. The initial weight increase frequently stabilises with time, proper diet and exercising.
Diabetes Management
Avoid or Limit These Common Foods with Hidden Sugar
Some foods that may contain hidden sugars include flavoured yoghurt, granola bars, canned fruit in syrup, condiments like ketchup and barbecue sauce, flavoured coffee drinks, packaged sauces and dressings, certain breakfast cereals, and processed snacks. Diabetics should read the food labels and be extra cautious about ingredients to manage diabetes well.
